Young Australian of the Year state finalist!
It’s been a while since I’ve posted but I have some exciting news – I’m a state finalist for the Young Australian of the Year Awards!
I’m excited and honoured to be nominated amongst so many inspiring people. And looking forward to the presentation wed night.
It is great to see the YesToKalydeco campaign acknowledged after hours, months, and years of campaigning to see Kalydeco listed on the PBS. Special mention needs to go to Faye as well.
Thanks to the people that nominated me and thanks everyone for all the comments on my facebook recently. My facebook went absolutely crazy! It’s been a difficult year health wise and it’s been hard to keep in touch with friends, so it’s been great to hear from so many people. I really appreciate the support, all of the nice comments mean so much more to me than the award itself.
I am gradually getting better (from my blocked blood vessel above my heart) and I’m extremely lucky that I was on Kalydeco over the last year or so. As exercise and physio have been very difficult, Kalydeco is the only thing that has kept my lungs well and out of hospital. Without Kalydeco I feel like I would have been very close to needing a transplant by now.
I haven’t had the energy to post on my research blog (sorry if you are a subscriber!), although I’ve still been posting on facebook (and I’ve been busy starting WeNeedOrkambi), but I’m hoping to get back to blogging soon. I’ll keep posting updates here as well, although since January I haven’t had lung function numbers or much to post about! The only new thing has been my sweat test results this year – 47 and 46 – exciting to see Kalydeco continue to keep me below the CF diagnosis point for 3 years now!
Amazingly stable after 2.5 years of Kalydeco!!
I am having another procedure for my obstructed blood vessel tomorrow, but thought I would write about how everything is going with kalydeco in the meantime.
In december kalydeco was finally listed on the PBS in Australia!!! This means I suddenly had much more free time, I didn’t know what to do with myself!! I’m joking, but it is nice to have the 10-15 hours per week back, and with the way my health has been it would have been hard to do much anyway.
As a result of the PBS listing I had another sweat test, which was 44 🙂
Before kalydeco it was 102, at 1 month it was 54 and at 7 months it was 40.
Despite my other recent health issues my lungs have been amazingly stable, with an FEV1 of 68% at my last appointment. It really is my magic blue pill!!
My bone density is normal and has actually increased slightly over the last few years, my liver and kidneys are normal and my diabetes is diet controlled as my sugar levels have improved over the last year (healthier carbs, smaller meals, alpha lipoic acid with large meals). One of my vitamin levels is high (vit E – 49 umol/L) and the other two vitamin levels are normal (vit D – 90nmol/L, vit A – 2.1 umol/L). My doctor decided to halve my vitabdeck dose and it is possible that my levels may be ok with no vitamins.
My current CF treatments include pulmozyme, occasional ventolin, creon forte, a reflux medication, azithromycin, a vitamin & kalydeco. I have taken cipro occasionally and had IVs twice in the last 2.5 years, one time for my sinuses (which turned out to be the blocked blood vessel) and the other time was after south america / to maximise my health on kalydeco. This means I have not needed any IVs due to being unwell since being on kalydeco, compared to needing 3-4 admissions per year for the last 20 years. I have also not needed other nebulisers or chest physio since being on kalydeco, saving hours of time each day. I cough occasionally but seem to be clearing my lungs on my own without treatments.
This is my very exciting lung function graph showing how stable I have been for the first time in my life:
The small drop in 2013 was from my south america trip and the slightly lower numbers in 2014 were most likely affected by my inability to exercise and also to blow lung function tests properly. The peak in June 2014 was following IVs.
My weight dropped with the vein issue but I have plateaued now:
I will update soon hopefully with good news following the procedure.
16 December Update
I meant to update much sooner but the headaches made this difficult. Thanks to everyone who has sent me messages over the last month or so, sorry if I have not replied, I do appreciate all the supportive comments 🙂
Following my last update I had a CT and MRI of my head which showed that there wasn’t something else causing my headaches. I was discharged from emergency with pain relief and a plan to continue Warfarin (blood thinner) for 3 months.
I also found out that there was a clotting disorder in the family, and I was tested for these, and it turns out I have a Factor V Leiden mutation (5% of people have this). This means I am 8 times more likely than normal to have a clot. In combination with the pill (which increases the chance of a clot by 3-4 times) this means I am 35 times more likely to have a clot. I have now stopped the pill as the risk is too high, especially with things like picc lines or port tubing in my veins.
I have now been on blood thinners for 7 weeks and I think the headaches are about the same. There are good days and bad days so it is hard to say exactly but I still need panadeine forte daily. Some days I need endone when the headaches are particularly bad. The other neurological symptoms have improved (difficulty thinking/focussing, difficulty with short term memory) but I still notice these daily. I still feel a very strong pressure/discomfort with bending over, this has not improved if anything I think it is worse now.
Overall this means I have basically been lying in bed or sitting in bed most of the day, with brief activity but I have not been able to do anything useful like uni work.
It was hoped that I would have improved more by now (just over 1/2 way through the 3 months of planned Warfarin), so I am having balloon dilatation of my superior vena cava tomorrow. It is thought that there may be a clot in a stenotic/narrowed area of my SVC. The balloon dilatation will hopefully widen this so blood can flow through again to my heart. Several of these procedures may be needed and I may still need blood thinners. I am currently in hospital waiting for the procedure tomorrow so I will try harder to update sooner than last time!
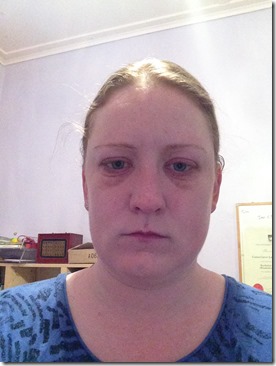
I have added some photos below showing my puffy face since April:
The swelling varies a little, sometimes it has been mostly my eyes, sometimes my whole face, sometimes my neck.
This is what I normally look like, taken January this year.
4 November Update
Sorry to those who have sent messages that I haven’t answered, I’ve been on strong pain relief over the last week.
The infusaport removal went well, following this the angiogram showed nothing had changed and that the vein (superior vena cava or SVC) is still completely blocked.
I have had problems with severe dizziness, headaches, difficulty focussing/thinking and difficulty with my short term memory over the last week, which I believe is related to an increase in intracranial pressure (from the vein blockage). I have mentioned these symptoms to my doctor and they are hopeful that the warfarin will soon help if there is a clot in the narrow SVC. Overall my symptoms have not improved since before I had the infusaport removed.
I have been very reliant on pain relief and frustratingly have now run out of the stronger meds (confusion since last week with faxing scripts to my pharmacy that appear to have gone missing). Wasn’t able to get an appointment with my GP and tried to organise seeing another GP but the wait was over an hour and I didn’t have the ability to wait in a chair that long.
Whilst I am expressing my frustration I’ll also add that it is frustrating that I’ve had this blockage since April but it was missed, with doctors not thinking about other options, and I believe not taking what I was saying seriously (in terms of the significant effect on daily activities/worsening symptoms and me questioning whether it was dental/sinuses). I am very grateful that it was finally picked up.
My parents were quite concerned so am now in emergency waiting to see someone, to try to get stronger pain relief and also to get a head CT and neurological consult.
Will update soon.
Below is the angiogram from last week, the blockage is just below the black area. It should flow straight down and into my heart, and instead is going around via the vein behind.
Just a few minor health issues…
I’ve been trying to do this blog post for a few days but my health has been making it hard. The last post took me even longer, even though I was mostly copying 🙂
Since March I have been having ongoing health issues. It started with needing many teeth fillings, and then a root canal. I had cheek swelling near that tooth. At the end of April I started feeling a pressure behind my eyes/cheeks, along with swelling around my eyes, which the doctors thought was sinusitis related to the tooth infection. I had various oral antibiotics, and then steroids, and then IVs, everything helped a little but nothing fixed the problem.
From June I noticed that this swelling and pressure was worse with exercise like tennis or skiing or movements like bending over. I would have good days and then without realising it would do something that meant the swelling and pressure became worse. From late August I started getting headaches as well and there were less good days.
By the end of September I had seen 7 medical professionals – CF doctors, ENT doctors, an endodontist and a dentist. Both the dentist and endodontist did not think my teeth were contributing to the current situation. At clinic they still thought it was related to my teeth and sinuses though, despite what the dentists thought & my emphasis on the severe impact this was having on my ability to do anything and how it was getting worse.
By October I had swelling (worse in AM), head pressure and headaches daily, with codeine needed on most days. I was not able to attend university or really do that much at all. I often felt like I had a concussion – hard to think/focus, headache, head pressure and tired.
I spoke to another CF doctor who suggested it may not be sinuses and it was worth doing tests to see if there was a blockage at the end of my infusaport. I googled this – Superior Vena Cava Syndrome – and found that I had pretty much every symptom listed there, and no symptoms that weren’t listed. I was booked in for an angiogram, to see if there was any narrowing of my SVC.
The angiogram was very conclusive – my SVC is completely blocked. This is how blood from the upper half of the body, including the arms and head, drains into the heart. This blood is instead travelling by a different vein (azygos) down to my abdomen, and then back up through the inferior vena cava to the heart. Basically doing a loop via my stomach bypassing the blockage. It is why I have a back up of fluid in my face (swelling around eyes, neck, face), head pressure/headaches/difficulty thinking (cerebral edema) and fatigue. It is also why lying flat, bending over and any exercise has a sudden increase in head pressure often leading to an increase in headache.
The fatigue is different to what I have experienced with CF & lung infections. I often feel suddenly tired, and I can’t push through it, the only option is to lie down and rest. It makes sense to me now, I am used to being able to push through being tired, but it just hasn’t been possible. There is only so much the cardiovascular system can do if there is back up of fluid in the top half of the body.
I am shocked and amazed to see that such a major vein is completely blocked, and yet the body has found a way around this. The doctors think that my infusaport tubing became tethered to the side of the vein, potentially due to it moving up and down slightly, leading to my SVC becoming narrow / collapsing, possibly with a clot. The infusaport still flushes normally, but has always been temperamental in terms of taking blood.
It seems likely that the dental issues did cause some swelling in March/April, and then around the same time swelling from my narrow SVC also started. Having two issues at the same time meant that the second one wasn’t picked up for a while, and means I have had this issue since at least April. I have had the infusaport since June 2012, so it is possible it has been developing for a while.
I am having the infusaport out today, and will be on blood thinners for 3 months. If there is a clot it is hoped this will allow the vein to return to normal, otherwise surgical options may be needed. I am hopeful that removing the infusaport as well as the blood thinners will help my symptoms soon, but aware it may take a while.
I will post again soon, hopefully with good news 🙂
The picture on the right is what I have:
More information, if anyone wants to read about SVC syndrome: http://www.nlm.nih.gov/medlineplus/ency/article/001097.htm
CFSA Ball Speech
Just a quick update to say my lungs are going well but I have had some other health issues, will write more in another blog post. Hopefully soon 🙂
In the meantime I thought I would add my speech from the recent CFSA ball:
Hi everyone, my name is Gen, and I’d like to share my story about living with Cystic Fibrosis.
I was diagnosed with CF at the age of 3. I was too young to understand what this meant, but it was a massive shock to my parents as nobody knew CF could be in the family. Back in 1989, my parents were heartbreakingly told that my life expectancy was mid to late teens.
Straight away this meant I needed to take many tablets each day, spend an hour a day with chest physiotherapy and have regular check ups at the hospital. My health was reasonable at first, but it got worse as I got older, and I started needing regular hospital admissions. I missed weeks of school at a time, due to chest infections, my digestive system, and even a stroke at the age of 7.
During high school my health declined, despite spending 6 to 8 weeks a year in hospital for my lungs, and having overnight feeds from the age of 12, in an attempt to help me gain weight. This was also when I realised what CF meant, as I saw many of my friends, who were the same age as me, becoming sick. Sadly many passed away. I hoped that I was a long way from needing a lung transplant, but my uncertain future and the realisation that I was not going to live as long as my friends was impossibly hard to accept as a teenager.
I worked hard to catch up work throughout high school, often to the detriment of my health, and through determination achieved a year 12 score of 99.6. This was then followed by uni, where I studied Biomedical Science, and then Physiotherapy. Despite my health continuing to decline, I was in the top 15% of both of these degrees.
I knew that a transplant may not be far away, so I always tried to do as much as possible whilst I was still well enough. This lead me to study in England, work as a ski instructor, teach English to children in asia and to travel and see as much of the world as possible.
My lung function continued to get worse and in 2012 it reached a very low 41 percent. To put this in perspective 30 percent is commonly when transplant is discussed. By this stage, I had been admitted to hospital over 60 times, which meant I had spent more than 3 years of my life in hospital.
I reached the point where I was puffed out with basic things like walking, spent hours a day on never ending treatments, and struggled to keep up with work and uni. I was very worried that my health would get worse with even a simple cold. At this point I was extremely fortunate to start a revolutionary medication called Kalydeco, which treats the underlying CF defect, helping 8 percent of people with CF.
The change with this medication was astonishing, within weeks I was back at 70 percent and my health was stable for the first time in my life. I stopped needing regular hospital admissions, and I have now been out of hospital for over 2 years, which is a 20 year record for me.
Kalydeco has allowed me to do things that I never thought I would be able to do, like visiting Machu Picchu, at a very high altitude, with no breathing issues whatsoever. Kalydeco has also changed my life expectancy significantly. I can now stop worrying that a transplant, or a life threatening chest infection is around the corner and instead think about having children and my career as a physiotherapist. I even need to think about superannuation.
The amazing changes that I’ve experienced first hand highlight the importance of research. Whilst I have been very lucky, sadly I have lost too many friends to CF, many that were younger than me. The reality is that for 9 out of 10 of my friends, there is no Kalydeco yet. We need research to occur as quickly as possible, which is one of the key areas that CFSA aims to support.
I feel extremely fortunate to have benefited from this amazing break through, in fact it feels like I’ve won the lottery, and I can be excited about the future for the first time in my life. And it’s with your help, that I hope my friends can grow old with me.
My family
#YesToKalydeco Campaign goes to Canberra
Happy 65 Roses Day everyone!
I plan to write an update about my health soon, but in the meantime I thought I would write about the Kalydeco situation in Australia.
Kalydeco is still not available in Australia, due to lengthy price negotiations between Vertex and the Australian Government. These negotiations first started over a year ago. This means Australia is now over two years behind the US and over one year behind the UK and Europe in terms of Kalydeco access.
We need Vertex to lower the price and we need the Australian Government to compromise on price. We need this to happen now.
For the last two years I’ve been very involved with #YesToKalydeco Campaign on both facebook and twitter. Many of us behind the campaign met for the first time in person in Canberra last Wednesday. Cystic Fibrosis Australia organised two events, a morning tea and evening cocktail event, aiming to raise awareness about Cystic Fibrosis & the urgent need for Kalydeco.
So after a very rushed birthday (I think I will celebrate this later when Keith is back from his trip to the middle of nowhere), I flew to Canberra for these events. It was an action packed day, with a morning tea, where we all met each other for the first time, spoke to several MPs about Kalydeco & heard from Peter Dutton the Health Minister, followed by a meeting with the senior advisor to the shadow Health Minister, then finding out that I was giving a speech that night, quickly writing my speech in about an hour, getting to the cocktail event and almost collapsing as I had a hypo pre speech (skulled some soft drink and luckily made it through!). The speech went really well, I was glad that I could let Peter Dutton know exactly how I feel regarding the Kalydeco situation, for a full 3 minutes!! It was also great talking to several other MPs that night, especially Senator Anne Urquhart & MP Ken Wyatt.
I’m sure the MPs that were present came away from these events understanding the urgency behind the PBS listing of Kalydeco. I’m very hopeful that we will hear the outcomes from recent meetings between Vertex and the health department in the near future & that soon they will agree on a price.
A real highlight for me was meeting everyone for the first time in person, after working together with the campaign for over 2 years!! I hope the next time we see each other is at a celebratory Kalydeco party!
Please support the #YesToKalydeco Campaign by following us on twitter and facebook, and also signing our petition. We need as much support as possible!
I have added a copy of my speech that I presented in Canberra below. I spoke at Parliament House to the Minister of Health, Peter Dutton, several other MPs and members of the CF community:
Hi everyone, my name is Genevieve Handley and I have been extremely fortunate to have been on Kalydeco for almost 2 years, through the Vertex compassionate program.
Before I started Kalydeco my health was hugely unstable and my lung function was 41%. To put this in perspective 30% is commonly when transplant is discussed.
I struggled to keep up with work and uni, and had to spend up to 2 hours a day on exhausting, never ending, treatments.
For 20 years I had about 3 hospital admissions a year. This meant I had over 60 hospital admissions, equalling more than 3 years of my life in hospital.
Amazingly, Kalydeco has allowed me to stay out of hospital for almost two years now. This is a 20 year record for me. For the first time in my life my health is stable and my lung function is 70%.
I now spend less than 5 minutes on treatment per day, saving many hours per week. I am back at uni and planning to start working soon.
Kalydeco has allowed me to do things that I never thought I would be able to do, like visiting Machu Picchu, at a very high altitude, with no breathing issues whatsoever. Even recently, I have had some non CF health issues, but thanks to Kalydeco, my lungs have been stable. Previously, I would be in hospital, probably on oxygen, potentially not recovering.
Before Kalydeco I rarely thought further ahead than 5 years, in fact I rarely even committed to events for the weekend, as I did not know if I would be well.
Kalydeco has changed my life expectancy significantly. I can now stop worrying that a transplant, or a life threatening chest infection is around the corner and instead think about having children, my career, I even need to think about superannuation!
Having experienced what Kalydeco can do first hand, I know exactly how important it is that the 200 patients in Australia access Kalydeco now. Every day the decision is delayed, people are getting sicker. This is urgent, I have lost too many friends to CF, most in their 20s.
Peter Dutton and Members of Parliament, our lives are in your hands. Without Kalydeco we will die prematurely. Currently 90% of eligible patients in the world outside Australia have access to Kalydeco. Kalydeco is available in the US, UK and majority of Europe. Yet, Australia, a country which prides itself in being one of the most developed in the world, has not approved Kalydeco. We need you to make a difference, please do everything you can to help the 200 Australians to access Kalydeco.
————————
Some photos from Wednesday:
Naomi, Faye, Rachelle, myself and Leah, five of the many passionate people behind #YesToKalydeco
Great turn out from the Cystic Fibrosis community at the morning tea event in Canberra
Presenting my speech at Parliament house. To my left is the Health Minister, MP Peter Dutton and Senator Anne Urquhart, to my right are MP Ken Wyatt, Mitch Messer, CFA President & Michelle Skinner, CFA CEO. I would like to sincerely thank Senator Urquhart & MP Ken Wyatt for hosting the events, as well as Senator Urquhart for organising for me to give a speech at the cocktail event. It is great to see politicians supporting Cystic Fibrosis and #YesToKalydeco.
1000 magic blue pills
Decided to update my blog after 6 months of neglect!
Since I last blogged I have been skiing, 4wdriving, finished uni placements and exams, visited Kangaroo Island, went to the Australian Open tennis & have been quite involved with the Kalydeco campaign in Australia. I was also interviewed by a TV program about the current delay regarding Kalydeco availability in Australia: 730 Report Story
Last September I also had my first IVs on Kalydeco. We decided that after 1 year of Kalydeco, given that I used to have IVs every 3-4 months, that it made sense to use IVs to get my lungs in the best shape possible. I had also dropped very slightly to 66% after visiting South America.
After two weeks I was at 69% and my cough had decreased significantly (less sputum, lighter green, thinner). I didn’t feel that different, but my varying energy levels are more related to CF diabetes.
In September I also started taking insulin (fast acting with meals high in carbohydrate), however I have had numerous issues with what may be an allergy to the insulin. It has been quite painful to inject, we are still working on this, and potentially may try tablets (although generally tablets are not the preferred CF treatment option). When I have injected insulin it has worked well; my energy levels improve significantly and I feel less tired after eating.
I have also had ongoing issues with reflux and possibly gastritis recently. Always fun waking up at 4am with a stabbing pain in your stomach!
So overall the lungs are going amazingy well, still stable after almost 1.5 years of Kalydeco. I find it hard to believe (as it is just so different to before) how little my lung function varies, mostly staying betwen 69-70. I have never been this stable, especially with no physiotherapy and minimal medications. However, I am having reasonable issues with the diabetes in particular, but it is not surprising given that I am 28. Hopefully this will improve soon.
Photos from my ski trip last September at Perisher:
Keith and I on the chairlift
Updated graphs:
The CF Rollercoaster Ride
Just like a rollercoaster, my health has had ups and downs over the last 28 years.
Kalydeco has helped my lungs significantly; my FEV1 has been stable at close to 70% for one year and I have only had IVs once in the last year, a 20 year record.
However I noticed that my energy levels have not matched my new lung function. My energy levels have improved, but not to the same extent that I have heard about with others on Kalydeco. Although I have been attending university much more often, and completing subjects unlike last year, I have struggled to keep up at times. In particular I have often felt tired in the afternoons and evenings.
I assumed this was normal CF tiredness. I think I’ve been tired since about 2008. This seems normal to me, I really cannot understand people who jump out of bed in the morning. And who aren’t tired. To me this seems very abnormal.
I came back from South America and my lungs were slightly below my new baseline of 70%. We decided it was time for my first IVs for two reasons 1) I had dropped slightly to 66% and 2) I still have pseudomonas in my lungs and have not had IVs yet, so it made sense to try IVs to get my lungs in the best possible shape.
I decided it would also be a smart idea to monitor my blood sugar levels. I have had impaired glucose tolerance since 2001, with OGTTs between 11 and 15. This means I have been pre-diabetic for about 12 years. For the last few years my self monitored blood sugar levels were 8-9 after meals on average and insulin was not needed. I am supposed to monitor these sporadically and generally have done this when on IVs.
After monitoring my blood sugar levels for a few weeks, I noticed they are higher now. I am about 10-12 on average after a reasonable size meal. Below about 8 is normal. I noticed that when I am high (above about 9), I feel tired. Sometimes I also had a headache. I realised that this potentially fits with what has been happening all year, I have often felt tired after lunch and dinner, and in April-May I had frequent headaches late evening.
I had another OGTT and this time it was 22. I felt terrible, first I was high, very tired, and basically could not function and use my laptop. Then 5 hours later I was down at 2.4 and felt terrible as I was really low. This is reactive hypoglycemia, with CF diabetes my insulin response is delayed, so I often get high and then low. I first felt reactive hypoglycemia in 2006.
So how does this relate to the rollercoaster? Well I feel that my lungs have been pretty much ‘fixed’ for now. I hoped that CF diabetes might be avoided (along with other CF complications) now that I’m on Kalydeco. Sadly this has not happened, and it appears that the CF diabetes has been having a pretty significant impact on my energy levels. I have just started taking insulin, I am hoping this will help.
Kalydeco & Cystic Fibrosis Diabetes:
My doctor mentioned that they had heard that blood sugar levels could vary more once on Kalydeco. I looked back through my named patient program information and found that it was suggested that close monitoring of blood sugar levels was needed, as high and low blood sugar levels can occur. I have heard anecdotally that some people have needed to increase their insulin dose after starting Kalydeco or that their blood sugar levels have increased. However, I have also read a recent article that suggests that Kalydeco may help increase the amount of insulin (and hence decrease the blood sugar levels). At this stage this is based on a very small study, it will be interesting to see the results of larger studies. In my case I was in the pre-diabetic category for many years, so it is not surprising that I am now diabetic. I hope those who start at a young age/before significant damage can avoid these types of complications.
Interesting Info:
– Recent research suggests almost half of those with CF will develop diabetes by age 30.
– Recent research also suggests that few people with CF have normal glucose metabolism. It is thought that all CF patients with pancreatic insufficiency have a degree of endocrine insufficiency (ie decreased insulin), however many CFs still have near normal glucose metabolism as their pancreas can compensate.
Almost one year of Kalydeco
Decided it was time for a summary post about my new health on Kalydeco.
I have been on Kalydeco for 11 months through the Named Patient Program, a program where Vertex supply Kalydeco to those who are very unwell. Kalydeco is the first medication that treats the underlying cause of Cystic Fibrosis in patients with the G551D mutation.
Before Kalydeco my lung function was 41% and very unstable. I was in hospital every 3-4 months. I was on medications that treated the CF symptoms; these were becoming less effective as I grew older.
For the last 11 months my FEV1 has been stable at approx 70%. This is amazingly stable compared to before; for 20 years my lung function has varied up to 20% from month to
month, now I am stable for the first time in my life. This is my highest in 3 years.
I have stayed out of hospital for 11 months, which is a 20 year record (I am currently on IVs for mostly prophylactic reasons, I will post about this soon). Before Kalydeco I had over 60 hospital admissions, equalling 3 years of my life.
Every aspect of my health has improved with Kalydeco, I have gained 6kg, I can run up stairs, I can sleep without coughing and I’m attending uni more often. My sweat test results have improved from 102 to 40. This is much lower than the point (60) associated with the CF diagnosis.
Previously I did not plan further ahead than 5 years. At the age of 28, with a life expectancy of 37, I knew transplant was edging closer. Thanks to Kalydeco I now don’t have to plan around hospital and CF, instead I can plan to have a family, a career and to grow old with my lungs.
I hope that Kalydeco can become available to everyone around the world who may benefit as soon as possible. Kalydeco is not approved in Australia yet; we are trying to speed up the reimbursement process and would appreciate your support on facebook and twitter.
Images from Dec 2011 and May 2013. Inflammation and scarring appear white, this has improved significantly on my second xray.